
100+ Providers Trust
Minnesota's TOP OB/GYN Medical Billing Company
Precise CPT/ICD Coding, Denial Management, and Timely Payment Posting with Our Full-Service OB/GYN Billing Company
-
98% of claims approved first submission
-
Structured follow-ups shorten AR by 30%
-
97% of previously denied claims recovers fast
-
Payments process 20-25% faster on average

Let’s get in touch
Please fill up the form, one of our AAPC certified medical biller and coder will reach out to you.
Inefficiencies Costing You Thousands? Here's How Our OB/GYN Billing Service Fixes That Fast

Full Adherence to Regulations
All Minnesota Medicaid, HIPAA, and payer-specific rules are strictly followed for accurate, error-free, fully compliant claims processing.

Efficient Payer Coordination
Expert handling of all payer contracts, rules, and requirements delivers maximum reimbursements with zero compliance risk.

Denial Root Cause Mapping
Patterns behind denials get tracked and corrected upstream so recurring mistakes no longer cause revenue to be lost

Maximum Revenue Capture
Specialized OB/GYN processes combined with smart monitoring deliver 20% faster reimbursements and 25% higher collections.

Pre-Billing Quality Checks
Claims are reviewed for missing data, documentation gaps, and coding errors before submission to minimize denials.

Post-Billing Revenue Analysis
Systematic review of finalized claims identifies payment gaps, inefficiencies, and opportunities to maximize revenue potential.
Our Success in Numbers
10 YRS
in Business
96%
Claim Success
$0 M
Claim Processed
33%
Reduction in AR
Get Paid Faster and Smarter with Us
Most practices think they're compliant, until payments are denied. BillingFreedom reviews every code, record, and gap so Minnesota OB/GYN practices finally get paid for every service they provide.
Run a Stronger, More Profitable Practice with Our Expertly-Managed OB/GYN Billing Service Support
Structured Accuracy Checks on Every Claim and Code Submission
You've heard it all before: "Specialized OB/GYN billing!" "We'll handle everything!" Then you watch the same companies make coding errors and act shocked when half come back denied. That's where a trusted OB/GYN billing service makes the difference. We dig into every detail like payers could zoom in at any second because sometimes they do. Blue Cross, HealthPartners, Medica, UCare, PreferredOne review every claim with a microscope. Every modifier, every date, every missing signature. We do too. We double-check that 59400, 59510, 59610, 59618 global packages actually have the full antepartum, delivery, AND postpartum documentation (spoiler: most don't). We make sure shared visits don't get bundled wrong, multiple gestations get the right modifiers without over- or under-billing, and anything outside the global package is documented separately and accurately for full reimbursement. We review every claim against payer edits, sequencing rules, and medical necessity requirements specific to Minnesota. The result? fewer avoidable rejections, faster turnaround in accounts receivable, and more actual revenue collected.

Maximum Revenue Capture With Zero Payment Delays
Another EOB shows up 45 days late… again. Another "allowed amount" that's mysteriously $200 short and nobody noticed. Another patient statement that sat in someone's spam folder for three weeks. It's not bad luck. It's bad billing. BillingFreedom fixes it. Electronic payments are handled as soon as we get them. Underpayments are identified quickly, and appeals are submitted with proper documentation. Patient statements are professional, sent fast, and we actively follow up on unpaid balances. We make sure we meet Minnesota's filing deadlines: Medical Assistance, MinnesotaCare, all the managed care plans with their ever-changing rules. We know exactly when commercial insurers are legally supposed to pay under prompt-pay statutes… and we remind them when they conveniently "miss" the deadline by a week or three. Fair denials? We challenge them. Over time, your AR days decrease and clean claim percentages climb. Minnesota OB/GYNs who've made the switch are collecting more reliably and stressing less about cash flow. You're still watching the same slow drip while they're getting ahead. Feels normal to keep going like this?

Certified OB/GYN Billers and Coders in Minnesota
Are You Maximizing Revenue From Each Encounter? Let Our Experts Help
Your Minnesota practice remains financially strong and well-covered. We thoroughly check every visit, service, and chart entry to ensure OB/GYN coding is dead-on accurate and defensible. CPT and ICD-10 codes selection align perfectly with what Minnesota payers require so claims land clean, compliant, and ready to get paid without unnecessary delays.

Stabilize Your Revenue Streams with Our Smarter, Faster, Fully Managed OB/GYN Medical Billing Service
-
HIPAA-compliant data management and reporting
-
Timely follow-ups speed approvals by 30-40%
-
Zero-pay & low-pay claims tracked & recovered
-
Average payment cycle shortened by 20-30 days
-
Visibility and transparency of every dollar earned
-
Profit margins increased by 15-25% in first quarter
Fully Managed OB/GYN Billing Services Aligned With Compliance Standards
Connect With Our Billing Expert Now
Our OB/GYN billing team triple-checks all coding details, documentation, and guarantees faster, full reimbursements for every visit and procedure.

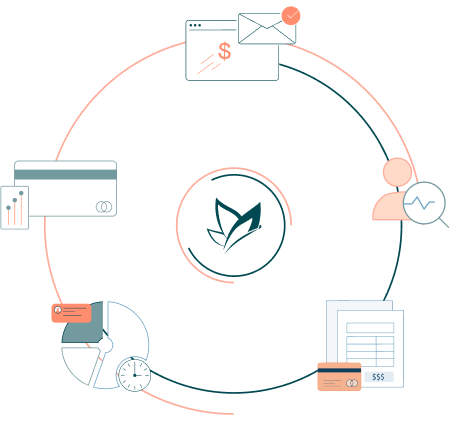
Each Stage of OB/GYN Billing Is Strategically Managed for Maximum Efficiency
Our team oversees every step of OB/GYN billing with full accountability: complete encounter checks, precise CPT/ICD-10 coding, immediate error fixes, reliable claim transmission to Minnesota payers, and clear visibility into what's paid, pending, or underpaid

Appointment scheduling

Patient Eligibility

Medical Coding

Claims Information

Claims Creation

Claims Scrubing

24 Hours Billing

AR Calling

Denial Management

EOB Posting

Clearing House

Claim Submission
Fully Compatible With Any EHR or EMR
Our Minnesota OB/GYN billing service works with whatever EHR or EMR your practice already has, no big changes needed. Practices in Minneapolis, St. Paul, Rochester, Duluth, Bloomington, and nearby towns have been using us for years for clean records, secure data handling, and higher revenue efficiency.
Drive Up Your Net Collections With Our OB/GYN Billing Services
Managing claims, coding, and payer requirements can pull your attention away from patients and mistakes cost money. The bigger risk is trusting a billing process you've never stress-tested. Payments accelerate when claims meet Minnesota payer rules the first time. We align CPTs with documentation, apply modifiers precisely, and submit complete clinical records so claims don't get questioned. Payers across the state value precision above all and that's precisely what our OB/GYN billing service provides. Solo providers, multi-physician groups, and women's health clinics statewide trust us to maximize net collections with zero added workload.
Connect with our billing specialist today. We'll review your billing history, expose revenue blind spots, and design a targeted plan to stop revenue leakage and stabilize your cash flow.
Let’s get in touch
Please fill up the form, one of our AAPC certified medical biller and coder will reach out to you.
Frequently Asked Billing Questions
Questions about OB/GYN billing? We handle coding details, submit claims properly, and get you paid on time so you can stop stressing about it. Reach out and see why we're the most trusted choice.


















