Accurate Eligibility and Benefit Verification Services
Improve reimbursements. Eliminate rejections and denials.

Insurance Eligibility Verification Services and Prior Authorization
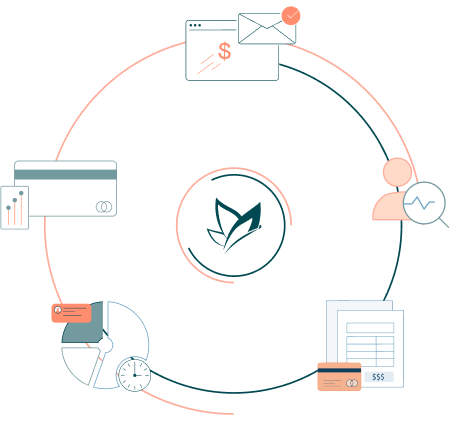
Set yourself up for success with automated eligibility and benefits verification services before medical service. Our experts carry out insurance verification and prior authorization checks as part of the billing process.

Coverage
Ensuring timely verification of patient coverage with all payer types, keeping patients’ accounts updated.

Benefits Options
We ensure patient information is updated, including payable benefits, deductibles and policy status.

Referral Authorizations
Identifying and documenting requirements of authorization or a referral to prevent revenue loss.

Accurate Documentation
Adequate and accurate documentation and recording of all benefits accurately to support seamless billing.

Deductibles, Co-pays, and Co-insurance
Ensuring the accurate estimate for patient deductibles amount, amount met, and co-pay or co-insurance.

Exceptional Workflow
Enhance patient outcomes and increase revenue with our optimized and efficient workflows.
Our Success in Numbers
10 YRS
in Business
98%
Claim Success
$0 M
Claim Processed
33%
Reduction in AR
Level-up your practice today!
See how Billing Freedom can help your practice grow and thrive in today’s modern healthcare era.
How We Support Your Success
Prevent Delays & Denials
Eligibility and benefits verification are critical first steps before submitting a claim to an insurance plan payer. Incorrect insurance eligibility verification remains one of the top reasons for claims being rejected, delayed, or denied. All these eligibility issues cause payment delays that directly impact the physician's office cash flow. Maintaining a solid insurance verification process within the practice can reduce these types of denials and make your practice more efficient with the improved bottom line; we at BillingFreedom ensure correct benefits verification and determine the correct amounts a patient may owe. Discover how, together, we can transform your business insightfully.

Realtime & Automated Eligibility Checks
Insurance verification involves many complicated and time-consuming steps, and sometimes, verifying patients’ insurance coverage can be challenging due to complex systems and inconsistent data. The patient’s insurance coverage eligibility must be checked before the patient’s appointment to accurately report demographic information on insurance claims. BF has extensive knowledge and experience with government insurance as well as commercial insurance. We provide comprehensive and customized insurance eligibility verification services for all medical specialties and practices of all sizes. Our services included end-to-end insurance eligibility validation prior to appointments determining out-of-network, thus helping practices to prevent accounts from aging and becoming uncollectable.

Eligibility & Benefits Verification Specialists
Accurate Verification, Faster Approvals, and Reduced Claim Denials
Prevent billing errors and claim denials with BillingFreedom’s Eligibility & Benefits Verification Services. Our certified billers and coders ensure real-time verification of patient coverage, deductibles, copays, and prior authorizations, helping providers avoid unexpected claim rejections. Optimize your revenue cycle with BillingFreedom.

Advanced workflows and scalable solutions. Drive by a team committed to your success.
-
Boost revenue by up to 35%
-
Cut bad debt and grow revenue
-
Solutions tailored to your practice
-
Certified billers and coders
-
Practice-Focused account executives
-
Data security you can trust
Billing Made Simple!
Supercharge your practice with modern, tech-enabled, and time-saving automations.

EHRs we work with
Medical billing company that knows the features and workaround of your EHR system. At BillingFreedom we work with your existing EHR.
What our clients say?


100+ Providers Trust
We switched from in-house billing to BillingFreedom year ago. The decision was difficult, but we definitely made the right choice. They cleaned up the mess caused by our previous biller. I would highly recommend BillingFreedom medical billing services. I would very much recommend BF to other OB/GYN’s.


Marguerite Brathwaite MD
Health Care Hospital


Ammar Wehbhe MD
Health Care Hospital


150,000 Providers Trust
We switched from in-house billing to BillingFreedom year ago. The decision was difficult, but we definitely made the right choice. They cleaned up the mess caused by our previous biller. I would highly recommend BillingFreedom medical billing services. I would very much recommend BF to other OB/GYN’s.


Marguerite Brathwaite
Health Care Hospital


Ammar Wehbhe MD
Health Care Hospital
Eligibility & Benefits Verification FAQ’s

Maximize Collections with Timely Benefits Verification for Your Practice
A well-executed Eligibility & Benefits Verification process helps healthcare providers avoid revenue losses and operational inefficiencies while ensuring a seamless patient experience. We at BillingFreedom focus our center our services towards perfecting your practice’s administration and ensuring maximum patient satisfaction.
Get in touch with one of our representatives for a detailed rundown and quote. You can receive a free virtual tour to figure out how our services can fine tune your practice’s revenue cycle.
Let’s get in touch
Please fill up the form, one of our AAPC certified medical biller and coder will reach out to you.








