Credentialing Services to Healthcare Providers
Planning to start a new practice: We credentialed you with several payers.

BillingFreedom Provider Credentialing Services.
We help you credentialed with all the major payers, insurance carries, and networks of your choice

Provider Enrollment & Credentialing
We rigorously work with payers to complete the enrollment and contracting process.

CAQH Credentialing & Maintenance
BF handles the creation, validation & maintenance of your CAQH profiles.

Re-Credentialing Services
Conduct all the re-credentialing services based on insurance policies and requirements.

Medicare & Medicaid Enrollments
Work as your advocate for Medicare & Medicaid enrollment. Both initial and renewal.

EFT Enrollments
Enroll with payers that allow for electronic transactions, such as EDI, ERA & EFT.

Contract Renegotiation
Let us handle the negotiations for you. Get the reimbursement you deserve.
Our Success in Numbers
10 YRS
in Business
98%
Claim Success
$0 M
Claim Processed
33%
Reduction in AR
Level-up your practice today!
See how Billing Freedom can help your practice grow and thrive in today’s modern healthcare era.
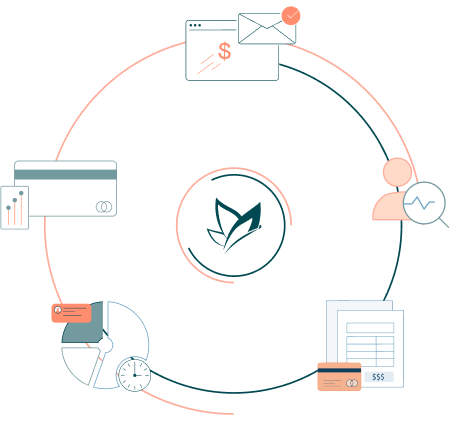
How We Support Your Success
Your Insurance Credentialing Experts:
Give your practice a competitive edge by working with an expert credentialing team for your office. We are the right choice when you want to credential a practice or add a payer. We have the expertise to maximize every dollar possible with our expert medical credentialing services. Whether you are a solo practice or a multispecialty group, we ensure that you’ll receive the best credentialing solution for your organization. We do everything: credentialing, enrollment processing, manager care contact, revalidations, and more. Our credentialing specialists are trained to navigate both credentialing and contracting to ensure providers are on the panels.

Let us handle the paperwork:
We process credentialing applications for healthcare providers so that they can bill health plans and receive in-network reimbursements without any delays. Whether you are a solo practitioner or large group practice, our deep experience working with the credentialing department of different payers across the United States ensures that you’ll receive the best of class credentialing support and solution for your organization. We take on the credentialing process right from scratch to finish. That means a lot of responsibility that would fall on the facility can be completed by the team BillingFreedom. When you outsource your medical provider credentialing to a group of experts, you limit the risk of potential revenue loss and improve the practice’s reputation overall.

Credentialing and Enrollment Professionals
Faster Approval,s Hassle-Free Setup, Compliance Assurance
Secure your practice’s financial stability with BillingFreedom’s Credentialing Services. Our certified experts handle the entire provider enrollment, payer contracting, and credentialing verification process, ensuring compliance with insurance networks and regulatory standards. Partner with BillingFreedom for a seamless credentialing experience today.

Eliminate revenue leakage with sophisticated billing solutions. Boost collections efficiently. Maximize revenue.
-
Boost revenue by 10-35%
-
Reduce write-offs and denials
-
Personalized support for your office
-
Faster processing, quicker payments
-
Real-time customized reporting
-
HIPAA-compliant, secure billing
Billing Made Simple!
Supercharge your practice with modern, tech-enabled, and time-saving automations.

EHRs we work with
Medical billing company that knows the features and workaround of your EHR system. At BillingFreedom we work with your existing EHR.
What our clients say?


100+ Providers Trust
We switched from in-house billing to BillingFreedom year ago. The decision was difficult, but we definitely made the right choice. They cleaned up the mess caused by our previous biller. I would highly recommend BillingFreedom medical billing services. I would very much recommend BF to other OB/GYN’s.


Marguerite Brathwaite MD
Health Care Hospital


Ammar Wehbhe MD
Health Care Hospital


150,000 Providers Trust
We switched from in-house billing to BillingFreedom year ago. The decision was difficult, but we definitely made the right choice. They cleaned up the mess caused by our previous biller. I would highly recommend BillingFreedom medical billing services. I would very much recommend BF to other OB/GYN’s.


Marguerite Brathwaite
Health Care Hospital


Ammar Wehbhe MD
Health Care Hospital
Frequently asked Credentialing questions
Unable to find an answer you’re looking for? No problem. Connect with a live person and we’ll work to get your question answered.

Seamless Credentialing with BillingFreedom
Streamline your healthcare practice with our expert credentialing services, ensuring swift provider enrollments and hassle-free insurance network participation. BillingFreedom simplifies the credentialing process, minimizing administrative burdens and accelerating approvals so you can focus on patient care. Our team handles every detail, from verifying provider credentials to managing payer contracts, reducing delays and ensuring compliance.
Schedule a quick virtual demo or connect with our credentialing specialists to see how we can support your practice’s growth. We’re available 24/7 to answer any questions. Contact us today, let’s simplify credentialing for your success!
Let’s get in touch
Please fill up the form, one of our AAPC certified medical biller and coder will reach out to you.








